Kyondrian
Uploaded by
y4c6pp7y6sKyondrian
Uploaded by
y4c6pp7y6sRISK ADJUSTMENT
TRAINING
Agenda
• Part 1:
• Revenue Cycle and Risk Adjustment Fundamentals
• Example
• Part 2:
• Specific HCC groups, with CDI tips to properly document and assign ICD 10
Guidelines
• V28 Update and what to expect
2
Part 1:
Risk Adjustment Fundamentals
Revenue Cycle
Patient Scheduling
and Registration
Insurance Eligibility
Credit Balance and Verification and
Patient collection Patient Co-Pay
Collection
RCM is the step-by-step lifecycle from
Payment processing when a patient first books an
and posting and Obtaining Previous
Denials Medical Records appointment until the practice receives
Management
full reimbursement for the claim.
Billing Audit process
and Claim CDI
submission
Patient encounter:
HCC Capture
4 (Assessment/Plan)
Medicare Risk Adjustment
Centers for Medicare and Medicaid Services
“Statistical process that takes into account the underlying health
status and health spending of the enrollees in an insurance plan
when looking at their health care outcomes or health care costs.”
Financial Perspective
Risk adjustment ensures that the plan is properly compensated for
the clinical burden of each member.
Risk Coders
Is about making sure the medical record accurately reflects the
diagnoses and procedures captured on a claim.
5
Risk Adjustment Fundamentals
CMS adjusts their monthly per capita payments to Health Plans considering the relative health
of their members; also known as “Risk Adjustment”
Risk Adjustment allows CMS to pay plans for the risk of the beneficiaries they enroll, instead
of an average amount for Medicare beneficiaries.
The payment that the health plan receives is based on member’s RAF/MRA score.
This is determined by diagnosis coding (ICD-10).
Risk adjustment is used to adjust bidding and payment based on the health status and
demographic characteristics of an enrollee.
[1]
to Congress: Medicare Advantage
Risk Adjustment - December
6 2021t to Congress: Medicare
Advantage Risk Adjustment -
December 2021
Risk Score/Risk Adjustment Factor (RAF)
• A risk score is the • The risk score of • RAF scores are • Health Plans
numeric value an an enrollee resets calculated to receive less
enrollee in a risk every January 1 estimate and payment for
adjustment and is officially predict the cost of healthier
program is calculated by the healthcare that members and
assigned each state or an organization more for sicker
calendar year government entity may have to bear members.
based on overseeing the in the future.
demographics risk adjustment
and diagnoses program the
(HCCs) member is
enrolled in.
7
Components of RAF score
8
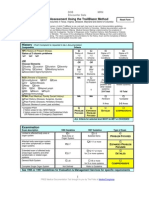
RAF Score Calculation
Demographics
Extra RAF:
0.155
HCC111:
HCC85:
Independent
COPD
CHF
County Rate
Hierarchical condition categories (HCC)
variables
Age
Sex HCC Interactions
Disability status
HCC Counts
Medicaid eligibility
Institutional status End Stage Renal Disease (ESRD Program)
9
Payment HCC count
HCC count provides additional
RAF Score whenever 4* or
more conditions are properly
documented and reported
within the same calendar year.
Adding a bonus in the
premium.
10
CMS-HCC Disease Interactions
Cancer HCCs Diabetes Mellitus (HCC 18) COPD (HCC 111)
HCC 47
CHF (HCC 85) CHF (HCC 85)
Disorder of immunity
Extra RAF: Extra RAF: Extra RAF:
0.838 0.121 0.155
COPD / Pulmonary Fibrosis CHF (HCC 85)
CHF (HCC 85)
(HCCs 111 -112)
Specified Heart arrythmias
CKD (HCCs 136 -138) Respiratory failure (HCC 84) (HCC 96)
Extra RAF: Extra RAF: Extra RAF:
0.156 0.363 0.085
11
Risk Adjustment Process
Data Collection Risk Score Payment Audit and
Calculation Calculation Compliance
• Medicare Advantage • CMS calculates a risk • CMS uses the risk • CMS conducts audits to
(MA) plans collect data score for each enrollee scores to adjust the ensure that MA plans
on the health status of based on their health payment rates for MA are accurately reporting
their enrollees. status data. plans. their enrollees' health
• Medical records, claims • The risk score reflects • Plans with sicker status data.
data, and health the expected healthcare beneficiaries receive • Plans that fail to comply
assessments. costs for that enrollee higher payments to with the reporting
relative to the average account for the higher requirements may face
Medicare beneficiary. expected healthcare financial penalties.
costs.
12
HCC: Hierarchical condition category
9,797 ICD-10 Map to
86 HCC Categories
an HCC
2020 V24 72,184 ICD-10 Codes
Model in Total
13
HCC: Hierarchical Condition Category
An HCC is a category of chronic medical conditions that share similar cost patterns, conditions organized
into body systems or comparable disease processes that Medicare correlated with increased cost of care.
Diabetes
without
Complication
(HCC 19)
HCC 85 HCC 11 HCC 40:
• I27.21: Secondary • C07: Malignant • M05.39: Rheumatoid Breast,
Prostate, and
pulmonary arterial neoplasm of parotid heart disease with Other
Cancers and
hypertension gland. rheumatoid arthritis Tumors (HCC
• I50.22: Chronic • C14.0: Malignant of multiple sites. 12)
systolic (congestive) neoplasm of pharynx, • M32.9: Systemic lupus
heart failure unspecified erythematosus, Diabetes with
Chronic
• I43: Cardiomyopathy • C15.9: Malignant unspecified Complications
(HCC 18)
in diseases classified neoplasm of • M34.9: Systemic
elsewhere esophagus, sclerosis, unspecified
unspecified Seizure
Disorders and
Convulsions
(HCC 79)
An ICD-10 code which risk adjusts maps to exactly one HCC, but not all ICD-10 codes map to an
HCC.
14
HCC Coding Fundamentals
SUBMITTING CODES: codes must be captured during face-to-face visits with the patient, by an
MD/DO, PA or APRN and it must be signed/closed in a period no longer than 30 days.
ACUTE CODES: Some Acute codes cannot be coded in primary care physician office (i.e., acute
CVA, acute pulmonary embolism, acute infarct).
ICD-10 > CODE FIRST/CODE ALSO: instruct that 2 codes may be required to fully describe a
condition.
ICD-10 > EXCLUDES: conditions that cannot be coded together.
15
New year, clean slate…
Each member’s risk score will reset to ZERO every year. (Jan 1st) What this
means is that on January 1st of every year each patient is “healthy”.
The diagnosis submitted to CMS the previous year WILL NOT carry over
and will have to be addressed in a physician office for the current
calendar year.
16
HCC Coding and Documentation
Specificity is key when it comes to HCC coding and documentation
A lot of the work for HCC
falls to the For HCC coding to be successful, the provider should strive
Coders/Auditors/CDI The goal is/has/and will to accomplish documentation standards by using MEAT:
Specialist, to ensure that always be to code to the
each patient’s medical
record is coded accurately
highest level of specificity,
for the success of the Risk M - Monitor signs and symptoms (disease process)
and that there is the proper
supporting documentation Adjustment process.
regarding the status of the
condition.
E - Evaluate (test results, medications, patient response to
treatment)
While most doctors A - Assess (ordering tests, patient education, review records,
Providers must report on document reasonably well counseling patient and family)
each patient’s risk for medical care, many are
unaware of the details
adjustment diagnosis, and needed for accurate code
it must be based on selection for billing, T - Treat (meds, therapies, procedure, modality)
clinical documentation. reimbursement, and quality
measure purposes.
17
MEAT Criteria – Provider
• Questions that a Healthcare Provider might consider when documenting
for a specific ICD-10 code using the MEAT criteria technique.
• Monitor:
1. What methods am I using to track this condition?
2. How often am I checking on this condition?
3. Are there any changes in the patient's condition since our last meeting? Self-reported by patient?
• Evaluate:
1. How am I checking if the treatment is working?
2. Have there been changes in the patient's condition since we last checked?
3. Is the patient showing a positive response to the current treatment?
• Assess/Address:
1. What is my overall view of the patient's health?
2. How am I dealing with any additional health issues related to this condition?
3. Do I need to involve any specialists to understand or manage this condition better?
• Treat:
1. What specific actions am I taking to help improve this condition?
2. How am I changing the treatment plan based on how the patient is responding?
3. How am I explaining the treatment to the patient, and how are they taking in this information?
18 [2]
Let’s go through an example!
Mrs. Jane lives in the state Florida. She resides in the city of
“Apple County” FL, which has a county rate of $1000. She is a
70-year-old female currently using a wheelchair who lives
at home and who is eligible for Medicare due to age.
Note:
Demographic conversion factor: 0.421
19
Code Assignment
ICD10 Code RAF Score added
E11.51: Type 2 diabetes mellitus with diabetic peripheral angiopathy without gangrene 0.302 + 0.288
I50.22: Chronic systolic (congestive) heart failure 0.331
I20.9: Angina Pectoris 0.135
F20.9: Schizophrenia, unspecified 0.524
F03.90: Unspecified dementia without behavioral disturbance 0.346
Z89.431: Acquired absence of other right toe(s) 0.519
Total 2.444
Extras RAF Score added
Demographic conversion factor 0.421
HCC Interaction (Diabetes + CHF) 0.121
HCC Count (6 HCC Conditions) 0.126
Final Total 3.112
20
RAF Score Calculation
In return for taking on the financial liability associated with the healthcare costs of Mrs. Jane for one month,
the Federal Government will be compensating her Medicare Advantage insurer following this formula:
•$1000 (County Rate) x 3.112 (total RAF score) = $3112/per month
21
Another example…
Let's pretend that Mrs. Jane's physician didn’t capture all her
chronic conditions, and risk codes were not submitted.
Her premium would be:
$1000 x (0.421 for demographic factor alone)= $421
$3.112 vs $421
Two different payments, yet medical
Six months of lost payment we
expenses to be covered remain the same
can NEVER recapture, assuming
and we are locked into that rate for at least
this patient is only seen once a year.
6 months.
22
Part 2:
Most common codes for chronic
conditions:
HCC 85: Chronic Heart Failure
Most Common Codes
ICD 10 Code Description
HCC 85 – RAF Score= 0.331 Code
I11.0 Hypertensive heart disease with heart failure
HCC 85 Total of 61 ICD 10 codes I13.0 Hypertensive heart and chronic kidney disease with heart failure and
stage 1 through stage 4 chronic kidney disease, or unspecified
chronic kidney disease
I13.2 Hypertensive heart and chronic kidney disease with heart failure and
Documents to review: with stage 5 chronic kidney disease, or end stage renal disease
• Echocardiogram I27.20 Pulmonary Hypertension, unspecified
• Cardiology records
I27.21 Secondary Pulmonary Hypertension
• ER/ED records.
I42.X Cardiomyopathy
I43 Cardiomyopathy in diseases classified elsewhere
I50.22 Chronic Systolic (Congestive) Heart Failure
I50.32 Chronic Diastolic (Congestive) Heart Failure
I50.9 Heart Failure, unspecified
25
Heart Failure
There are 2 main categories of Heart Failure
Systolic
I50.2- Occurs when the ability of the heart to contract decreases.
Diastolic
I50.3- Occurs when the heart has a problem relaxing between contractions
(diastole) to allow enough blood to enter the ventricles.
Fifth characters further specify whether the heart failure is
unspecified, acute, chronic, or acute on chronic.
[3]
26
I50.22: Chronic Systolic (Congestive) Heart Failure
To properly support
EF<55% reported on ECHO CHF Systolic diagnosis
Clinical findings and Plan/Treatment in all visits to keep
record consistency
is required to
•Other Names: document:
•HFrEF: Heart Failure with reduced ejection fraction Review Specialist records to locate the specific description
and status of the disease to assign the most appropriate
•Heart failure with Low EF code.
•HF with reduced systolic function
Echocardiogram review should be reported for support.
Diagnosis Criteria
Code Also:
E26.1: Secondary Hyperaldosteronism, when CHF is being
treated with chronic diuretics drugs (Loop diuretics and/or
Spironolactone). These codes should be linked and reported
together.
Acute vs Chronic: Clear and concise clinical documentation
reporting acute exacerbation or decompensation of chronic
heart failure even if mild, should be in the date of service
where this code is captured if applicable.
27 CDI tip: when the EF is at this level, I50.22
should be recommended
I50.32: Chronic diastolic (congestive) heart failure
Diagnosis Criteria
EF>55% reported on ECHO Grade I (impaired relaxation): This is a normal finding and occurs in
nearly 100% of individuals by the age of 60 years. Normal atrial
• Other Names: pressures. NOT ENOUGH TO SUPPORT I50.32 CODE.
• HFpEF: Heart Failure with preserved Ejection Fraction
• HF with preserved systolic function Grade II (pseudo normal): This is pathological and results in elevated
left atrial pressures. Presence of structural heart disease such as left
To properly Documentation of clinical findings and Plan/Treatment should be in atrial enlargement, left ventricular hypertrophy or systolic dysfunction.
support CHF all visits to keep record consistency
Systolic GRADE II + POSITIVE FRAMIGHAM CRITERIA: I50.32.
diagnosis is
required to Review Specialist records to locate the specific description and
status of the disease to assign the most appropriate code. Grade III (reversible restrictive): This results in significantly elevated left
document:
atrial pressures. Also known as a “restrictive filling pattern”
Echocardiogram review should be reported for support.
Grade IV (fixed restrictive): This indicates a poor prognosis and very
Code Also: elevated left atrial pressures. Diuresis will not have a major effect on the
E26.1: Secondary Hyperaldosteronism, when CHF is being treated
with chronic diuretics drugs (Loop diuretics and/or left atrial pressures, and clinical HF is likely permanent. Grade IV
Spironolactone). These codes should be linked and reported diastolic dysfunction is present only in very advanced HF
together. .
28
Framingham Criteria
Patient should meet:
• 2 MAJOR CRITERIA or
• 1 MAJOR CRITERIA & 2 MINOR CRITERIA
Common Diagnostic Tests:
• EKG
• Echo
• B type Natriuretic Peptide (BNP)
• Stress Test
Nature of Heart Failure can be:
• Systolic
• Diastolic
• Combined Systolic and Diastolic
[4]
29
NYHA: New York Heart Association HF Classification
-Document clinical findings for each date of service that
is pertinent to the episode of care.
-Additionally, make sure to include a specific assessment
and plan for the diagnosis to properly validate it.
[5]
30
ECHO EXAMPLE: Systolic CHF
31
CODE ALSO: Combination codes
✓ When coding for hypertension, congestive
heart failure and chronic kidney disease,
ICD-10 assumes a causal relationship
between hypertension and these two
conditions.
✓ The combination code for hypertensive
heart disease/kidney disease should be
used instead of the essential (benign)
hypertension code (I10).
The only time these combination codes should
not be used is if the provider states somewhere
in the medical record that the hypertension is
unrelated to the congestive heart failure or
chronic kidney disease, or if the provider states
that the congestive heart failure or chronic
kidney disease is due to another condition
besides the hypertension.
32
Pulmonary Hypertension
CDI Tips PH Classification
Group 1: Idiopathic, heritable, due to drugs and toxins, or
RVSP > 35mmHg or associated with conditions such as connective tissue diseases,
congenital heart disease, portal hypertension, and others.
<35 with impressions by Cardiologist stating PHTN
Group 2: Left-heart related PH.
• It is important to document the treatment for pulmonary
hypertension (PHTN) whenever a patient is receiving it. Even if the Group 3: Due to chronic respiratory disorders.
right ventricular systolic pressure (RVSP) is currently within normal
limits, documenting the medication will properly support PHTN. Group 4: Chronic thromboembolic PH;
[6]
Group 5: Multifactorial mechanisms, including: Hematologic
disorders such as Myeloproliferative disorders Splenectomy;
systemic disorders such as Sarcoidosis and pulmonary
Langerhans cell histiocytosis; Metabolic disorders, etc.
33
Other secondary PH
I27.20: Pulmonary hypertension, unspecified
34
I27.21: Secondary pulmonary arterial hypertension
This code includes secondary PAH
-Due to drugs or toxins.
-Underlying conditions such as congenital heart disease
-HIV
-Lupus polymyositis
-Portal hypertension due to advanced liver disease
-Rheumatoid arthritis
-Schistosomiasis
-Sickle cell disease
-Sjogren syndrome, and systemic sclerosis.
35
Other secondary PH: I27.2-
36
I27.0: Primary pulmonary hypertension
37
HCC 96
Specified Cardiac Arrhythmias
Most Common Codes
HCC 96 – RAF Score= 0.268 ICD 10 Code Code Description
I47.1 Supraventricular tachycardia
HCC 96 Total of 14 ICD 10 codes
I47.9 Paroxysmal tachycardia, unspecified
I48.0 Paroxysmal Atrial Fibrillation
Documents to review:
I48.11 Longstanding persistent atrial fibrillation
• EKG/Holter
• Echocardiogram I48.20 Chronic Atrial Fibrillation
• Cardiology records
I48.91 Unspecified Atrial Fibrillation
• Previous PCP records
• ER/ED records. I48.92 Unspecified Atrial Flutter
I49.5 Sick Sinus Syndrome
I49.5: Sick
39 Sinus Syndrome
Code Also: Z95.0 Presence of cardiac pacemaker, if applicable
I48.XXX: Atrial Fibrillation and Flutter
CDI Tips:
• EKG/Echocardiogram report
• Clinical findings in Physical Exam, if relevant to
episode of care
• Review Specialist (Cardiology) consult notes to locat
e the specific description and status of the disease t
o assign the most appropriate code.
• Medication reconciliation with Cardiology specialist
records should be performed to update active
prescriptions.
Atrial fibrillation or flutter + CHADVASC = 2 or higher:
Code also: D68.69: Other thrombophilia [Secondary
Hypercoagulable State], and document preventive long-term
Anticoagulant treatment. If patient is not on preventive
Long-term
40
Anticoagulant treatment document reason.
D68.69: Other thrombophilia [Secondary Hypercoagulable
State] (HCC 48)
Long term use of an
anticoagulant such
Secondary hypercoagulable state: as Coumadin, Eliquis,
Xarelto, And Pradaxa.
Acquired disorders that predispose
patients to thrombosis.
These involve blood flow
abnormalities or defects in blood
composition and of vessel walls.
D68.69, can be also coded with:
[7] -Pulmonary embolism (history of)
- Deep venous thrombosis (history
of)
- Valve replacement (not biological)
41
HCC 88: Angina Pectoris
Most common codes
HCC 88 – RAF Score= 0.135 ICD 10 Code Code Description
I20.1 Angina Pectoris with documented spasm
HCC 88 Total of 35 ICD 10 codes I20.8 Other forms of angina pectoris
I20.2 Refractory angina pectoris
Common records to review: I20.9 Angina pectoris, unspecified
- Cardiology reports
- ER/ED records I25.111 CAD with angina pectoris with documented spasm
- Previous PCP records. I25.112 CAD with refractory angina pectoris
I25.118 CAD with other forms of angina pectoris
I25.119 CAD with unspecified angina pectoris
43
Angina Pectoris
To Clinical findings in ROS/Physical Exam, if
properly relevant to episode of care In order to validate angina codes, the patient should be on:
support -Nitroglycerine
Angina Review Specialist consult notes to locate -Isosorbide
Pectoris the specific description and status of the
disease to assign the most appropriate c -Long-lasting antianginal medication (Metoprolol)
it's
ode.
required to
document:
Medication reconciliation with Cardiology • If any other medication is used to control angina,
specialist should be performed to update it should be documented.
active prescriptions that ensure angina • Medication needs to be refilled at least once a
codes are not resolved. year.
44
Refractory Angina Pectoris
• New Codes for 2023:
Refractory angina (RA) • I20.2: Refractory angina pectoris
Chronic condition (≥3 months) characterized by
• I25.112: Atherosclerosis heart disease
angina in the setting of coronary artery disease of native coronary artery with refractory
(CAD), which can not be controlled by a angina pectoris
combination of optimal medical therapy,
angioplasty or bypass surgery, and where • I25.702: Atherosclerosis of coronary
reversible myocardial ischemia has been clinically artery bypass graft(s), unspecified, with
established to be the cause of the symptoms. refractory angina pectoris
[8]
45
HCC 88 and HCC 87
HCC 88: Angina Pectoris HCC 87: Unstable Angina
• It occurs when the heart muscle doesn't get as much Unstable angina is an intermediate state between angina
blood as it needs. pectoris of effort and acute myocardial infarction.
• This usually happens because one or more of the
The most common cause is reduced blood flow to the heart
heart's arteries is narrowed or blocked, also
muscle causing injury to the coronary blood vessel. This results in
called ischemia. blood clotting, which blocks blood flow to the heart muscle.
[9]
The patient's pain is more acute, longer lasting, and more frequent
than angina, and more resistant to antianginal treatment.
Unstable angina may be documented as accelerated, crescendo,
pre-infarction, or intermediate coronary syndrome.
“AHA Guidelines recommend initial treatment of Unstable
Angina in the ED/ER” Unstable angina is a MEDICAL EMERGENCY and requires
acute care hospitalization.
This
46 codes should not be reported in the PCP setting.
HCC 108
Vascular Diseases
Most Common Codes
HCC 108 – RAF Score= 0.288 ICD 10 Code Code Description
I70.0 Atherosclerosis of Aorta
HCC 108 Total of 330 ICD 10 codes I70.1 Atherosclerosis of renal artery
I70.201 Atherosclerosis of native arteries of extremities, right leg
Common records to review: I70.202 Atherosclerosis of native arteries of extremities, left leg
• CXR
I70.209 Atherosclerosis of native arteries of extremities, unspecified extremity
• CT Scans
• MRI I71.2 Thoracic aortic aneurysm, without rupture
• Ultrasounds I71.4 Abdominal aortic aneurysm, without rupture
• Other imaging studies.
I73.9 Peripheral vascular disease, unspecified
Wording commonly used: I77.1 Stricture of artery
• Dilation I77.810 Thoracic aortic ectasia
• Calcified plaque
I82.501 Chronic embolism and thrombosis of unspecified deep veins of right lower
• Atherosclerosis extremity
• Aneurysm
I82.502 Chronic embolism and thrombosis of unspecified deep veins of left lower
• Ectasia extremity
• Stenosis
Tortuous.
• 48
I73.9: Peripheral vascular disease, unspecified
Clinical findings that must be documented:
• Intermittent claudication (pain or discomfort in the lower extremities and buttocks that occurs with
exercise/activity and resolves with rest)
• Diminished pulses in legs or feet
• Decreased blood pressure in the affected limb(s)
• Arterial bruits(a whooshing sound heard with a stethoscope over the artery)
• Ulceration and sores with poor healing
• Hair loss on the legs and feet
• Discoloration of skin (bluish, dusky)
• Decreased warmth in the lower extremities
[10]
Does the patient have any complementary
NO studies, such as US Duplex Arterial/venous YES
ultrasound, XR, etc.?
Continue coding I73.9 since there is no ABI, Doppler Arterial US, Angiogram, Venous Doppler ultrasound consistent
specific diagnosis or cause and consider CXR Showing narrowed/blocked with condition affecting venous vessels
ordering additional imaging to obtain a vessels, decreased flow, or
more accurate diagnosis. atherosclerosis
”Advised to wear compression
stockings, limit sodium intake
and elevate BLE, RTC if Remove I73.9 and continue coding Remove I73.9 and continue coding
symptoms worsen"
more specifically, depending on the more specifically, depending on the
This is not proper
documentation, according to the location and severity of the condition, location and severity of the condition,
guidelines, since this description for example: for example:
is not documenting the -I70.201: Atherosclerosis of native -I87.2: Venous insufficiency (chronic)
condition, it is documenting the
managing. arteries of extremities with intermittent (peripheral)
49 claudication, right leg. -I83.1: Varicose veins of lower
extremities with inflammation
CDI Tips
• I73.9: Peripheral vascular disease, unspecified; • In Diabetic patients with
• Documentation of clinical findings in Physical Exam, in all visits to keep angiopathy (E11.51) the ICD10
record consistency classification presumes a causal
• Review Specialist (Vascular) consult notes to locate the specific description and relationship between the 2
status of the disease to assign the most appropriate code.
conditions linked by these terms
• Medication reconciliation with Vascular specialist should be performed to in the alphabetic index or tabular
update active prescriptions that ensure chronic thrombosis codes
are not resolved. list.
• Special studies that support these conditions include: • These conditions should be
• QuantaFlo/ABI coded as related unless the
• Arterial Ultrasound documentation clearly states the
• CTA conditions are unrelated.
• MRA • Thus, I70.XXX codes are
• Applicable to: included in the diabetic codes
• Intermittent claudication description and shouldn’t be
• Peripheral angiopathy NOS separately coded.
• Spasm of artery
• Excludes:
50 • Atherosclerosis of the extremities (I70.2-I70.7-)
HCC 84: Cardiorespiratory Failure
HCC 111: COPD
HCC 112: Fibrosis of lung and other chronic lung disorders
Most Common Codes
ICD 10 Code Description HCC
Code
HCC 111 – RAF Score= 0.288
J41.0 Simple Chronic Bronchitis 111
HCC 112 – RAF Score= 0.219
J42 Unspecified chronic bronchitis 111
HCC 84 – RAF Score= 0.282
J43.9 Emphysema, unspecified 111
J44.0 COPD with (acute) lower respiratory infection 111 HCC 111: Total of 15 ICD 10 Codes
J44.1 COPD with (acute) exacerbation 111 HCC 112: Total of 81 ICD 10 Codes
J44.9 COPD, unspecified 111 HCC 84: Total of 27 ICD 10 Codes
J47.9 Bronchiectasis, uncomplicated 112
J84.10 Pulmonary fibrosis 112
Common records to review:
J84.9 Interstitial pulmonary disease, unspecified 112
CXRAY, CT, PFT, Pulmonology Records,
D86.0 Sarcoidosis of lung 112
ER/ED Records.
J96.10 Chronic respiratory failure, unspecified whether with hypoxia or 84
hypercapnia
J96.11 Chronic respiratory failure with hypoxia 84
J96.12 Chronic respiratory failure with hypercapnia 84
52
HCC 111: COPD
• J44.0: COPD with (acute) lower respiratory infection,
CDI Tips Code Also to identify the specific infection.
• Clinical findings in Physical Exam, in all visits to keep
record consistency. If COPD is suspected based on findings
from the history and physical examination – it must be • J44.1: COPD with (acute) exacerbation, exacerbation
confirmed by spirometry to detect airflow obstruction. The shouldn’t be assumed based upon worsening of a
ACP, GOLD, and NICE guidelines emphasize clinical suspicion concomitant respiratory disease or when COPD is
of COPD based on history and physical examination findings, described as end stage.
with confirmation by Spirometry (PFT).
• A ratio of the forced expiratory volume in one second to Code Also: to identify Tobacco exposure, for example:
forced vital capacity (FEV1/FVC) less than 0.7 confirms the • Z77.22: Exposure to environmental tobacco
diagnosis of COPD. Seen in PFT [11] smoke
• Z57.31: Occupational exposure to tobacco smoke
• Z87.891: History of tobacco dependence
[11]
• F17.X: Tobacco dependence
• Z72.0: Tobacco use
53
Importance of Imaging Studies
Diagnostic tools are important when supporting/validating diagnosis codes. These are some examples on coding
opportunities found in CXRAY or PFT.
• From PFT:
• From Chest Xray: • HCC 111:
• J44.9: Chronic obstructive pulmonary
• HCC 111: disease, unspecified
• J43.X: Emphysema • J44.1: Chronic obstructive pulmonary disease
• HCC 112: Fibrosis of lung and other with acute exacerbation, episode of
exacerbation (needs to be reflected in DOS).
chronic lung disorders • J43.X: Emphysema
• J84.10: Pulmonary fibrosis, unspecified
• J41.0: Simple chronic bronchitis, is a clinical
• Other HCC 108: Vascular Disease diagnosis that doesn't require a specific
• I70.0: Atherosclerosis of aorta test, but clinical findings need to be
• I71.4: Abdominal aortic aneurysm, without
reported each time the code is being
rupture (removed if repaired) addressed to keep record consistency.
• I77.1: Stricture of artery (tortuous aorta) *This code is falls into HCC 111 as well*.
• I77.810: Thoracic aortic ectasia
[12]
54
HCC 112: Fibrosis of lung and other chronic lung
disorders
• CDI Tips
• Clinical findings in Physical Exam, in all visits to keep
record consistency. Findings reported in imaging • J84.XXX: Other interstitial pulmonary diseases,
studies should be referred to in the A/P when code is
being documented. Code first underlying disease, poisoning due to drugs or
• Review Specialist consult notes to locate the specific
toxins and/or additional codes for adverse effect to
description and status of the disease to assign the m identify drug when applicable.
ost appropriate code.
• Medication reconciliation with Pulmonology specialist
should be performed to update active prescriptions
55
HCC 84: Cardiorespiratory Failure
• CDI Tips
• Review Specialist (Pulmonology) consult notes to locate the
specific description and status of the disease to assign the most
appropriate code. • Chronic respiratory failure is very common in
• Cardio or Respiratory condition that requires them to be on patients with severe COPD and other chronic
oxygen (condition must be coded in the same encounter to lung diseases such as cystic fibrosis and
properly report interaction). pulmonary fibrosis.
• Plan of care with specification of the use of continuous • The most important tip-off to chronic respiratory
supplemental oxygen therapy (24/7). failure is chronic dependence on supplemental
• Code Also: Z99.81: Dependence on supplemental oxygen oxygen.
when reporting chronic respiratory failure.
• If patient refuses Oxygen, do not use Z99.81, but code for
Z91.19: Patient’s noncompliance with other medical treatment
[13]
and regimen, and document patient refuses Oxygen despite
medical indication.
56
HCC 18: Diabetes with Complications
HCC 19: Diabetes without Complications
Most Common Codes
ICD 10 Code Code Description HCC
HCC 18 – RAF Score= 0.302
E11.21 Type 2 diabetes mellitus with diabetic nephropathy 18 HCC 19 – RAF Score= 0.105
E11.22 Type 2 diabetes mellitus with diabetic chronic kidney disease 18
E11.311 Type 2 diabetes mellitus with unspecified diabetic retinopathy with macular edema 18
HCC 18: Total of 400 ICD 10 Codes
E11.36 Type 2 diabetes mellitus with diabetic cataract 18
HCC 19: Total of 6 ICD 10 Codes
E11.39 Type 2 diabetes mellitus with other diabetic ophthalmic complication 18
E11.40 Type 2 diabetes mellitus with diabetic neuropathy, unspecified 18
Common records to review:
E11.41 Type 2 diabetes mellitus with diabetic mononeuropathy 18
E11.42 Type 2 diabetes mellitus with diabetic polyneuropathy 18
Foot exam, CMP, HbA1C, ABI,
E11.51 Type 2 diabetes mellitus with diabetic peripheral angiopathy without gangrene 18 108
E11.621 Type 2 diabetes mellitus with foot ulcer 18
E11.69 Type 2 diabetes mellitus with other specified complication 18
E11.65 Type 2 diabetes mellitus with hyperglycemia 18
E11.649 Type 2 diabetes mellitus with hypoglycemia without coma 18
E11.9 Type 2 diabetes mellitus without complications 19
Z79.4 Long term (current) use of insulin 19
58
Disclaimer
• E11.XX Group codes will be used to exemplify Diabetes with/without complication, appropriate
diabetes ICD 10 codes (E08.-; E09.-; E10.-; E11.-; E13.-) should be used for specific diabetic
patients.
• E08.XX: Diabetes due to underlying condition • E09.XX: Drug or chemical induced diabetes • E13.XX: Other specified diabetes mellitus,
Code first underlying conditions when applicable, such mellitus includes
as: Code first poisoning due to drug or toxin if applicable Diabetes mellitus due to genetic defect of Beta-
Congenital rubella (P35.0) (T36-T65) cell function
Cushing syndrome (E24.X) Use additional code for adverse effect if Diabetes due to genetic defect in Insulin action
Cystic Fibrosis (E84.X) applicable to identify drug (T36 – T50) Post-pancreatectomy diabetes
Malignant neoplasm (C00-C96) Use additional code to identify control using: Post-procedural diabetes
Malnutrition (E40-E46) Insulin (Z79.4) Secondary diabetes NEC
Pancreatitis and other diseases of the Oral antidiabetic/hypoglycemic drugs
pancreas (K85.X – K86.X) (Z79.84) Use additional code to identify control using:
Use additional code to identify control using: Insulin (Z79.4)
Insulin (Z79.4) Oral antidiabetic/hypoglycemic drugs
Oral antidiabetic/hypoglycemic drugs • E10.XX: Type 1 diabetes mellitus, code group (Z79.84)
(Z79.84) includes:
Brittle diabetes When Post-procedural or Post-pancreatectomy
Diabetes due to autoimmune process hypoinsulinemia (E89.1) is documented with
Diabetes due to immune mediated pancreatic Post-procedural or Post-pancreatectomy diabetes
islet Beta-cells destruction (E13.XX), code E89.1 should be sequenced first
Juvenile onset diabetes
Ketosis prone diabetes
59
Diagnosing Tools
1. TWO (2) consecutive Fasting blood sugars
greater than or equal to 126 mg/dL (90-180 A1C (Percent) Fasting Glucose
days apart) (mg/dL)
2. TWO (2) consecutive A1C greater than or
equal to 6.5 (90-180 days apart).
3. Both parameters altered on the same date, Diabetes 6.5 or above 126 or above
patient is automatically diagnosed
4. Glucose tolerance continues to be the Gold
Standard Prediabetes 5.7 to 6.4 100 to 125
ADA
Normal Around 5 or less 99 or below
[14]
60
Diabetes with Complications
CDI Tips
• E11.21: Type 2 diabetes mellitus with diabetic nephropathy, document altered histopathological study results.
• E11.36: Type 2 diabetes mellitus with diabetic cataract, Is a presumed causal relationship unless provider states that is due to a
different cause. If Age related cataracts diagnosis is seen in Eye note, provider must document that cataracts are related to
diabetes if applicable. Once cataracts are removed consider resolved and delete.
• E11.649: Type 2 diabetes mellitus with hypoglycemia without coma, Fasting Glucose <70mg/dl, sugar levels and treatment
must be reported at time of diagnosis.
• E11.65: Type 2 diabetes mellitus with hyperglycemia characterized by HbA1C levels greater than 8% or multiple fasting
glucose levels exceeding 180mg/dl. This condition requires appropriate treatment to regulate blood sugar levels, but it does
not qualify as uncontrolled diabetes.
• E11.69: Type 2 diabetes with other specified complication, complication should be linked with wording
• Code also: E78.5: Hyperlipidemia, unspecified: Documentation must link lipid disorder to Diabetes ("Diabetic Dyslipidemia", "due to diabetes", "in diabetes", "Diabetes with
Dyslipidemia")
61
-E66.01: Morbid (severe) obesity due
to excess calories (Acute).
-N52.1: Erectile dysfunction due to
disease classified elsewhere. Must
document relationship between the two
conditions (chronic).
-E78.2: Mixed hyperlipidemia or E78.5:
Hyperlipidemia, unspecified. Diabetic
dyslipidemia need to be established
(chronic).
62
Diabetes with Complications
CDI Tips
• Diabetic Complications that fall under 2 HCC groups:
• E11.22: Type 2 diabetes mellitus with diabetic chronic kidney disease – HCC 18 + HCC 136-138 Code Also: Stage of CKD (N18.2
– N18.6) [See next slide with Stages of CKD]
• E11.35XX: Type 2 diabetes mellitus with proliferative diabetic retinopathy – HCC 18 + HCC 122 [RAF: 0.524]
• Found in Ophthalmologist note, mentioning diabetic proliferative changes, macular edema and specifies affected eye, review
the note and find most specific code to report.
• E11.51: Type 2 diabetes mellitus with diabetic peripheral angiopathy without gangrene – HCC 18 + HCC 108 [RAF: 0.590]
• Needs proper testing to be accurate, such as: Arterial ultrasound of the extremities or arterial brachial index or X-ray of
extremity with findings of vascular calcification.
• E11.621: Type 2 diabetes mellitus with foot ulcer – HCC 18 + HCC 161
• Code Also: Site and Stage of Ulcer L97.—
• E11.622: Type 2 diabetes mellitus with other skin ulcer – HCC 18 + HCC 161
63 • Code Also: Site and Stage of Ulcer L97.--
ICD 10 CKD Stage GFR
N18.2 CKD stage 2, mild 60 – 89 ml/min/1.73 m2
N18.30 CKD3 unspecified Unspecified
N18.31 CKD stage 3a, moderate 45 – 59 ml/min/1.73 m2
N18.32 CKD stage 3b, moderate 30 – 44 ml/min/1.73 m2
N18.4 CKD stage 4, severe 15 – 29 ml/min/1.73 m2
N18.5 CKD stage 5, kidney failure < 15 ml/min/1.73 m2
End stage renal disease < 15 ml/min/1.73 m2 , requires chronic dialysis or
N18.6 (ESRD) transplant
To establish CKD: 2 GFR, 90-180 days apart **AA GFR
[15]
64
65
HCC 18: Neurological complications
<Presumed relationship per ICD-10>
CDI Tips:
• E11.40: Type 2 diabetes mellitus with diabetic
• E11.43: Type 2 diabetes mellitus with diabetic
neuropathy, unspecified
autonomic (poly)neuropathy, includes Diabetic
• E11.41: Type 2 diabetes mellitus with diabetic Gastroparesis and any other autonomic
mononeuropathy manifestations. Clinical documentation should
• E11.42: Type 2 diabetes mellitus with diabetic report all findings when the code is reported.
polyneuropathy.
• Document symptoms and clinical findings in physical exam, ICD 10 guidelines EXCLUDES the use of
annual foot exam or podiatry evaluation. Either present or G63 along with E08-E13.4X codes
improving with active medication.
• Once diagnosed with neuropathy, regular revisions during
examination is recommended (COA – Foot exam).
• Patients that have not been diagnosed with neuropathy
should be tested at least twice a year. [16]
66
• If a diabetic complication has been coded, E11.9 Diabetes without
complications should not be coded. In case E11.9 has already been
added to the problem list, it should be removed, and only the
specific ICD-10 code for the diabetic complication should be
reported. Such as:
• E11.42: Type 2 diabetes mellitus with diabetic
polyneuropathy
• E11.69: Type 2 diabetes mellitus with other specified
complication
• E11.51: Type 2 diabetes mellitus with diabetic peripheral
angiopathy without gangrene
67
E11.8: Type 2 diabetes mellitus with unspecified
complications
Diabetes with complications:
• E11.42: Type 2 diabetes mellitus with diabetic polyneuropathy
• E11.21: Type 2 diabetes mellitus with diabetic nephropathy
• E11.22: Type 2 diabetes mellitus with diabetic chronic kidney disease
• E11.51: Type 2 diabetes mellitus with diabetic peripheral angiopathy without gangrene
• E11.69: Type 2 diabetes mellitus with other specified complications
68
HCC 21: Protein-Calorie Malnutrition
HCC 22: Morbid Obesity
Most Common Codes
ICD 10 Code Description HCC HCC 21 – RAF Score= 0.455
Code
HCC 22 – RAF Score= 0.250
E44.0 Moderate protein-calorie malnutrition 21
E44.1
HCC 21: Total of 10 ICD 10 Codes
Mild protein-calorie malnutrition 21
HCC 22: Total of 7 ICD 10 Codes
E46 Unspecified protein-calorie malnutrition 21
R64 Cachexia 21 Common records to review:
E66.01
CBC/Protein levels, Kidney function,
Morbid (severe) obesity due to excess calories 22 Blood sugar levels, CXRAY, etc.
Z68.41 Body mass index (BMI) 40.0-44.9, adult 22
Z68.42 Body mass index (BMI) 45.0-49.9, adult 22
Z68.43 Body mass index (BMI) 50-59.9, adult 22
Z68.44 Body mass index (BMI) 60-69.9, adult 22
Z68.45 Body mass index (BMI) 70 or greater, adult 22
70
HCC 21: Protein Calorie Malnutrition
CDI tips E44.X/E46: Diagnosis criteria (2 or more of the following):
• BMI <19
• Document subjective and objective findings that
are consistent with the diagnosis of malnutrition. • Weight loss greater than or equal to 2% in one month, 5%
in 3 months, or 10% in 6 months.
• Specify the time frame and context that denotes • Unremitting, involuntary weight loss
the patient’s BMI decline.
• Be specific with the description of the diagnosis, • Serum albumin <3.5 (note that low albumin and pre-
such as severe, moderate, or mild malnutrition. albumin states alone are no longer considered diagnostic
• The diagnosis of malnutrition should be since these lab results are affected by inflammation).
consistent with an appropriate treatment and • Food intake severely reduced
follow-up plan. • Muscle wasting and fat loss: w/ presence of edema and/or
R64: Cachexia, ascites.
The condition is a symptom or side effect of chronic conditions, • All these findings must be properly documented on the
such as: encounter date where the ICD 10 is addressed to correctly
• AIDS validate it.
• Cancer
• Chronic obstructive pulmonary disease (COPD)
• Chronic renal failure
• Congestive heart failure Refer to: [17]
• Crohn's disease
• Cystic fibrosis GLIM Criteria
• Rheumatoid arthritis
Older individuals with "failure to thrive" syndrome may also
ASPEN criteria
develop cachexia.
• According to one study, an estimated 5 million Americans
71
have the condition.
HCC 22: Morbid Obesity
CDI tips <Patients might present PCM and
• BMI >40. Morbid obesity, they are not mutually
• BMI >35 + Applicable comorbidity such as: exclusive>
• Uncontrolled Hypertension (I10)
• Diabetes (HCC 18)
• Chronic Obstructive Pulmonary Disease (HCC 111)
• Coronary artery disease w/ or w/o angina (I25.XXX)
• Congestive Heart Failure (I50.XX)
• Peripheral Vascular Disease (I73.9-I70.2.-)
• Sleep Apnea (G47.X)
• Old Myocardial Infarction / Angina Pectoris (I25.2 –
I20.X)
Comorbidity must be properly documented, supported and linked [18]
to morbid obesity to meet this criteria
Code Also: Z68.XX Code to identify BMI.
72
HCC 23: Other significant endocrine and metabolic
disorders
Most Common Codes
ICD 10 Code Description HCC HCC 23 – RAF Score= 0.194
Code
E20.9 Hypoparathyroidism, unspecified 23 HCC 23: Total of 229 ICD 10 Codes
E21.0 Primary hyperparathyroidism 23
E21.1 Secondary hyperparathyroidism, not elsewhere
23
Common records to review:
classified Laboratory results, Specialist records.
E21.3 Hyperparathyroidism, unspecified 23
E22.X- Disorders of Pituitary gland and hypothalamic
E23X 23
dysfunction
E24.X Cushing’s syndrome 23
E26.1 Secondary Hyperaldosteronism 23
E27.X Disorders of adrenal gland 23
N25.81
Secondary hyperparathyroidism of renal origin 23
74
Hyperparathyroidism
CDI tips Hyperparathyroidism is often overlooked, and a PTH
• E21.1: Secondary Hyperparathyroidism, NEC; level should be ordered under the following
circumstances:
• E21.3: Hyperparathyroidism, unspecified; • Low Vitamin D levels
• Review Specialist/Endocrinology consult notes to locate the • High or Low Calcium Levels
specific description and status of the disease to assign the
most appropriate code. • CKD Stage 3 to ESRD
• Laboratory and imaging study reports to follow up and further
evaluate diagnosis. • N25.81: Secondary hyperparathyroidism of renal origin,
• If the primary cause of the endocrine disorder is successfully is associated to CKD 3 – ESRD
treated and resolved, switch to personal history code. • E21.0: Primary Hyperparathyroidism, is considered
• Genetic and special tests for metabolism disorders should be resolved after Parathyroidectomy procedure and should
uploaded to chart and refer to it at least once a year when be switch to personal history code.
recapturing the code.
• E20.9: Hypoparathyroidism, unspecified
• These codes are considered resolved when the laboratory
results are back to normal levels and should [19]
be removed/deleted. This criteria doesn’t include Secondary
Hyperparathyroidism of renal origin (N25.81)
75
E26.1: Secondary hyperaldosteronism
Diagnosis that meet criteria to use this codes with
conditions: HCTZ does not meet
▪ Congestive heart failure; criteria
▪ Severe Renal artery stenosis (>70%)
for this combination.
▪ Cirrhosis of liver with ascites, on the following
medication: Testing is needed when
• Loop diuretics: Bumetanide, Furosemide, Torsemide. combining E26.1 with any
• Aldosterone receptor antagonists: Spironolactone, other condition not listed
Eplerenone and Finerenone. here
[20]
76
CHF or
Cirrhosis or
Severe Renal artery
stenosis >70%
E26.1: Secondary
hyperaldosteronism
(HCC 23)
Furosemide or
Spironolactone or
Bumetanide
77
In patients with elevated homocysteine
levels in blood, DO NOT code E72.11:
Homocystinuria.
E72.11: Homocystinuria; inherited disorder of the metabolism of the amino
acid methionine due to a deficiency of cystathionine beta synthase or
methionine synthase.
Code instead R79.81: Abnormal findings of blood amino-acid level [21]
78
HCC 48: Coagulation defects and other specified
hematological disorders
Most Common Codes
ICD 10 Code Description HCC HCC 48 – RAF Score= 0.194
Code
D45 Polycythemia vera 48
D47.3 Essential (hemorrhagic) thrombocythemia 48 HCC 48: Total of 74 ICD 10 Codes
D57.3 Sickle-cell trait 48
D68.59 Other Primary Thrombophilia 48 Common records to review:
D68.69 Other Thrombophilia [Secondary
48 Laboratory results, ER/Hospital
hypercoagulable state]
records, Specialist records.
D69.2 Other nonthrombocytopenic (senile)
48
purpura
D69.6 Thrombocytopenia, unspecified 48
80
HCC 48: Coagulation defects and other
specified hematological disorders
CDI Tips:
• D47.3: Essential (hemorrhagic) • D69.2: Other nonthrombocytopenic
thrombocythemia: (senile) purpura:
• At least two (2) consecutive PLT count on CBC above Normal • Clinical findings should be documented on ROS and
values (450) and should be referred to Hematology to PE in every encounter to keep record consistency.
further evaluate and treat.
• D69.6: Thrombocytopenia, unspecified:
• D45: Polycythemia vera:
• LABS ARE NOT ENOUGH, needs further documentation • At least one (1) PLT count on CBC under
(bone marrow aspiration, oncology note, and/or JAK2 Normal values (150) and should be removed if
genetic testing) to be properly supported. PLT count returns to normal levels.
[22]
81
• D68.59: Primary Thrombophilia
• Primary or inherited hypercoagulable states VS • D68.69: Other Thrombophilia
• AKA: Secondary hypercoagulable state
• Applicable to:
• Applicable To:
• Antithrombin III deficiency • Hypercoagulable states NEC
• Primary hypercoagulable state NEC • Secondary hypercoagulable state NOS
• Primary thrombophilia NEC
• Protein C deficiency
• Protein S deficiency
• Diagnosis index:
• Hypercoagulable (state) D68.59
• Diagnosis index: • secondary D68.69
• Deficiency, deficient • specified NEC D68.69
• protein • Thrombophilia D68.59
• C - D68.59 • secondary NEC D68.69
• S - D68.59 • specified NEC D68.69
• Antithrombin - D68.59 (antithrombin III)
• Hypercoagulable (state) - D68.59
• antithrombin D68.59 (III)
• primary NEC D68.59
• protein C deficiency D68.59
• protein S deficiency D68.59 See Slide 41 for more information
• Thrombophilia D68.59
• primary NEC D68.59
82
HCC 57: Schizophrenia
HCC 59: Major depressive, bipolar and paranoid
disorders
Most Common Codes
ICD 10 Code Description HCC
Code
HCC 57 – RAF Score= 0.524
F20.81 Schizophreniform disorder 57
HCC 59 – RAF Score= 0.309
F20.9 Schizophrenia, unspecified 57
F25.9 Other schizoaffective disorders 57
HCC 57: Total of 74 ICD 10 Codes
F30.XX Manic episode 59
HCC 59: Total of ICD 10 Codes
F31.XX Bipolar Disorder 59
F32.X
Common records to review:
Major depressive disorder, single episode 59
ER/Hospital Records,
F33.XX Major depressive disorder, recurrent 59
Psychology/Psychiatry records, PHQ9,
R45.88 No suicidal self-harm 59
T14.91XX Suicide attempt 59
F30.XX – F31.XX – F32.X – F33.XX, they all
poses an EXCLUDES note, meaning that this
codes can’t/shouldn't be coded at the same
time [Coding Conflict]
84
HCC 59: Major depressive disorders
• F32.-Major Depressive Disorder, • F33.- Major Depressive Disorder,
single episode recurrent
• F32.0: MDD, single episode, mild • F33.0: MDD, recurrent, mild
• F32.1: MDD, single episode, moderate • F33.1: MDD, recurrent, moderate
• F32.2: MDD, single episode, severe without • F33.2: MDD, recurrent, severe without
psychotic features psychotic features
• F32.3: MDD, single episode with psychotic • F33.3: MDD, recurrent, with psychotic
features features
• F32.4: MDD, single episode, in partial • F33.40: MDD, recurrent, in remission,
remission unspecified
• F32.5: MDD, single episode, in full remission • F33.41: MDD, recurrent, in partial remission
• F33.42: MDD, recurrent, in full remission
• F33.8: Other recurrent depressive disorders
• F33.9: MDD, recurrent, unspecified
85 CDI Tips>Next Slide
F32.- MDD single episode F33.- MDD recurrent
• A single episode of a major depressive disorder lasts a • A recurrent depressive disorder is characterized by repeated
minimum of 2 weeks with persistent symptoms throughout episodes of depression without any history of independent
episodes of mood elevation and increased energy or mania. (At
the day. no time in the past has there been any hypomanic or manic
• An individual can only have 1 single depressive episode episodes.)
during his or her lifetime. • There has been at least 1 previous episode lasting a minimum
of 2 weeks and separated by the current episode by at least 2
months
• CDI TIPS:
• Depression screening test at least once a year to monitor condition
• Review Specialist records to locate the specific description and status of the disease to assign the most appropriate code and
to keep plan of care up to date
• Refer to DSM-5 guidelines for depressive, bipolar and paranoid disorders diagnosis.
• Depression codes shouldn’t be used along with Bipolar disorder codes. Use specific codes for mania/hypomania/depression in
bipolar disorder.
• To Assess Self-harm/Intentionality, review hospital records and/or psychiatry consult notes to keep record consistency, and
patient with positive answer on PHQ9 questions 3-5-9, please document suicide assessment on pertinent episodes of care.
• Description of Sequela of the self-harm if present, and documentation of Personal History of suicidal behavior (Z91.51).
86
[23]
F32.9: Major depressive F32.A: Depression,
disorder, single episode, unspecified
unspecified
• Always remember to “Code to the maximum level of specificity”, consider
reevaluating patient and find a more specific code like:
• F32.1: Major depressive disorder, single episode, moderate
• F33.0: Major depressive disorder, recurrent, mild
• F33.41: Major depressive disorder, recurrent, in partial remission
• F32.5: Major depressive disorder, single episode, in full remission
87
HCC 51: Dementia with complications
HCC 52: Dementia without complications
Most Common Codes
ICD 10 Code Code Description HCC HCC 51 – RAF Score= 0.346
F01.51X Vascular dementia, unspecified severity with behavioral
disturbance
51 HCC 52 – RAF Score= 0.346
F01.A1X Vascular dementia, mild 51
F02.81X Dementia in other diseases classified elsewhere, unspecified
51 HCC 51: Total of 70 ICD 10 Codes
severity, with behavioral disturbance
F02.B1X Dementia in other diseases classified elsewhere, moderate,
51
HCC 52: Total of 53 ICD 10 Codes
with behavioral disturbance
F03.91X Unspecified dementia, unspecified severity, with behavioral
51
disturbance
F03.C1X Unspecified dementia, severe, with behavioral disturbance 51 Must be supported by
G91.X Hydrocephalus 51 Imaging studies reporting
F01.50 Vascular dementia, unspecified severity, without behavioral positive findings
disturbance, psychotic disturbance, mood disturbance, and 52
anxiety
F02.80 Dementia in other diseases classified elsewhere, unspecified
severity, without behavioral disturbance, psychotic disturbance, 52
mood disturbance, and anxiety
Common records to review:
F03.90 Unspecified dementia, unspecified severity, without behavioral Previous PCP records, ER/Hospital
disturbance, psychotic disturbance, mood disturbance, and 52
anxiety Records, Specialist records
G30.X Alzheimer's disease 52
G31.XX Other degenerative diseases of nervous system, not elsewhere
52
classified
89
Dementia in other diseases Unspecified (senile)
Vascular dementia (Alzheimer’s/Parkinson’s) dementia F03.xxx
F01.xxx F02.xxx
4th Character
F0X.AO: Mild Dementia without
A: Mild
complications B: Moderate
F0X.BO: Moderate Dementia without
complications C: Severe
F0X.CO: Severe Dementia without
complications
WITH agitation: xxx.A11 WITH agitation: xxx.B11 WITH agitation: xxx.C11
WITH anxiety: xxx.A4 WITH anxiety: xxx.B4 WITH anxiety: xxx.C4
WITH mood disturbance: xxx.A3 WITH mood disturbance: xxx.B3 WITH mood disturbance: xxx.C3
WITH psychotic disturbance: xxx.A2 WITH psychotic disturbance: xxx.B2 WITH psychotic disturbance: xxx.C2
WITH other behavioral disturbance: xxx.A18 WITH other behavioral disturbance: xxx.B18 WITH other behavioral disturbance: xxx.C18
90
i.e., F03.C11: Severe senile dementia with agitation.
Dementia with and without Complications
CDI Tips:
• Clinical findings and behavioral disturbances when pertinent to episode
of care (MMSE)
• Review Specialist (Neurology) consult notes to locate
the specific description and status of the disease to assign
the most appropriate code.
• F01.XX: Vascular dementia without behavioral disturbance, should be
supported by imaging studies reporting vascular findings causing the
dementia.
• F02.XX: Dementia in other diseases classified elsewhere,
Code First underlying physiological conditions such as:
• G30.9 - Alzheimer's disease
• G10 – Huntington's disease
• G20 – Parkinson's disease
• G31.83 - Dementia with Lewy bodies
• G31.09 - Frontotemporal dementia
• G40.XX - Epilepsy and recurrent seizures
• S06.XX - Traumatic brain injury
And others.
[24]
91
Substance Use Disorder
HCC 54: SUD with psychotic complications
HCC 55: SUD, moderate/severe or substance use with complications
HCC 56: SUD, Mild [except Alcohol and Cannabis].
Most Common Codes
ICD 10 Code Code Description HCC
F10.131 Alcohol abuse with withdrawal delirium 54
HCC 54 – RAF Score= 0.329
F10.27 Alcohol dependence with alcohol-induced persisting dementia 54
HCC 55 – RAF Score= 0.329
F11.150 Opioid abuse with opioid-induced psychotic disorder with delusions 54
HCC 56 – RAF Score= 0.329
F12.151 Cannabis abuse with psychotic disorder with hallucinations 54
F13.951 Sedative, hypnotic or anxiolytic use, unspecified with sedative, hypnotic or
54
anxiolytic-induced psychotic disorder with hallucinations
HCC 54: Total of 116 ICD 10 Codes
F10.20 Alcohol dependence, uncomplicated 55
HCC 55: Total of 328 ICD 10 Codes
F10.21 Alcohol dependence, in remission 55
HCC 56: Total of 14 ICD 10 Codes
F11.120 Opioid abuse with intoxication, uncomplicated 55
F11.93 Opioid use, unspecified with withdrawal 55
F12.19 Cannabis abuse with unspecified cannabis-induced disorder 55
F12.280 Cannabis dependence with cannabis-induced anxiety disorder 55
F13.20 Sedative, hypnotic or anxiolytic dependence, uncomplicated 55
F14.120 Cocaine abuse with intoxication, uncomplicated 55
F11.10 Opioid abuse, uncomplicated 56
F11.11 Opioid abuse, in remission 56
F13.11 Sedative, hypnotic or anxiolytic abuse, uncomplicated 56
93
F14.11 Cocaine abuse, in remission 56
Substances capable of
inducing a disorder
• The DSM V recognizes substance-related disorders resulting from the
use of 10 separate substances:
[25]
• Alcohol (F10.-)
• Cannabis (F12.-)
• Hallucinogens (F16.-)
• Inhalants (F18.-)
• Opioids (F11.-)
• Sedatives, Hypnotics or Anxiolytics (F13.-)
• Stimulants (including amphetamine-type substances, cocaine
(F14.-), and other stimulants) (F15.-)
• Tobacco (F17.-)
• Other psychoactive substance (F19.-)
• Other or unknown substances
*Substance use disorder does not apply to caffeine
[26]
94
Substance Use Disorder (SUD)
CDI Tips:
• SUD clinical findings should be stated in pertinent episode of care and social history, describing pattern
of harmful usage (Dependence, Abuse or Use). DSM V Criteria
• Document current clinical status to ensure record consistency, and should be updated annually
(uncomplicated, intoxication, in remission, etc.)
• Specialist consult notes should be reviewed to identify the most appropriate code for the patient's
disease status.
• Counseling sessions should be documented, including the amount of time spent if relevant to the
episode of care.
• If rehabilitation therapy was discussed as a potential plan of care, it should be noted along with any
outcomes.
• For HCC 54: • For HCC 55 and 56:
• Document clinical characteristics of SUD with • Clinical characteristics of substance use disorder
psychotic complications, if present. and any related complications should be
• Include description of psychotic complications described when relevant to the episode of care.
and treatment/plan of care in documentation.
95 [27]
DSM V Criteria for
SUD
96
HCC 56
HCC 55
97
Alcohol Use Disorder (AUD)
The Audit C is commonly used to assess for Alcohol Use Disorder. If the results of the Audit C are positive, it may be
necessary to administer the CAGE Questionnaire to further evaluate the patient's condition
98
Alcohol Use Disorder (AUD)
Alcohol Dependence in Remission F10.21: Alcohol dependence in
remission.
• ICD-10-CM classifies a “history of” alcohol
abuse or dependence as in remission.
• The DSM-V defines remission as the
absence of any AUD diagnostic criteria
(other than craving/desire/urge for alcohol)
for at least three months.
99
Neoplasms/Cancers
HCC 8: Metastatic Cancer and Acute Leukemia
HCC 9: Lung and other severe cancers
HCC 10: Lymphoma and other cancers
HCC 11: Colorectal, bladder and other cancers
HCC 12: Breast, prostate and other cancer
Most Common Codes HCC 8 – RAF Score= 2.659
HCC 9 – RAF Score= 1.024
ICD 10 Code Code Description HCC HCC 10 – RAF Score= 0.675
C77.XX Secondary malignant neoplasm of lymph nodes 8 HCC 11 – RAF Score= 0.307
C78.XX Secondary malignant neoplasm of lung, liver and other digestive organs 8 HCC 12 – RAF Score= 0.150
C91.XX Acute lymphoblastic leukemias 8
C33.XX – C34.XX Malignant Neoplasm of Trachea, Bronchus and Lung 9
HCC 8 Total of 82 ICD 10 Codes
C90.0X-C90.2X Multiple Myeloma
Plasma Cell Leukemia 9 HCC 9 Total of 110 ICD 10 Codes
Extramedullary plasmacytoma
C92.1X - Chronic Myeloid Leukemia
HCC 10 Total of 534 ICD 10 Codes
C92.3X -
C92.9X -
Myeloid Sarcoma
9 HCC 11 Total of 133 ICD 10 Codes
Myeloid Leukemia, unspecified
C92.ZX
Other Myeloid Leukemia HCC 12 Total of 269 ICD 10 Codes
C40.XX – C41.XX Malignant neoplasm of bone and articular cartilage 10
C79.81
Secondary malignant neoplasms of breast 10
Common records to review:
C81.XX Hodgkin lymphomas 10
Previous PCP records, ER/Hospital
C82.XX-C86.XX Non – Hodgkin lymphomas 10
Records, Specialist records.
C18.X-C21.X Malignant neoplasms of large intestine, rectum and anus 11
C32.X Malignant neoplasms of larynx 11
DISCLAIMER:
C50.XXX Malignant neoplasm of breast 12 The codes provided here are only a portion of the
C61 Malignant neoplasm of prostate 12 HCC group, therefore, the most recent CMS ICD
D32.X
10 mapping should be referenced to identify the
Benign neoplasm of meninges 12
most precise and appropriate code
D35.X Benign neoplasm of pituitary gland, craniopharyngeal duct and pineal gland 12
101
CDI Tips
Every time any code is used, the plan of treatment (radiotherapy, chemotherapy, immunotherapy, hormonal adjuvant
therapy, surgery) is to be documented, if patient has completed treatment and there is no further evidence of
disease, it is appropriate to use a Personal History code (Z85.XX)
HCC 8
• Secondary Malignant neoplasms:
• Oncology records documenting the anatomic site, behavior, laterality and primary cancer type if possible.
• If primary malignancy has been successfully treated and there is no further evidence of active disease, Code First:
the secondary malignancy and assign a code from category Z85.XX to indicate the former site of malignancy as
secondary code.
• Acute Leukemias:
• Hematology/Oncology records supporting the diagnosis.
• Current treatment regime as specified on specialist note.
• The categories for acute leukemia have codes indicating whether the leukemia has achieved remission or not. If
the documentation is unclear as to whether the leukemia has achieved remission, provider should request
updated specialist notes and continue using active disease codes while pending confirmation.
• Document bone marrow transplant status (Z99.84) if applicable
102
CDI Tips
HCC 9 – HCC 10
• Behavior: malignant, neuroendocrine, carcinoma in situ, benign, or unknown.
• Metastasis (first code primary site then secondary cancer/metastatic site if applicable)
•If primary malignancy has been successfully treated and there is no further evidence of active disease, Code First: the secondary
malignancy and assign a personal history code from category Z85.XX to indicate the former site of malignancy as secondary code
• Review Hematology/Oncology consult notes to locate the specific description and status of the severe cancer to assign the most
appropriate code.
Continue using active/current diagnosis and documenting in the Assessment/Plan if patient:
• Is currently undergoing surgery, radiotherapy, immunotherapy, targeted therapy or chemotherapy, this should be reflected in
Plan/Assessment of Office visit to properly validate active diagnosis.
• Current Adjuvant therapy status post excision of the neoplasm, this should be reflected in Plan/Assessment of Office visit to
properly validate active diagnosis.
• Active surveillance, meaning that the Oncologist explained the different therapeutic options and the patient/caregiver refused any
treatment, thus the provider keeps the patient in active surveillance to evaluate the progress of the chronic disease.
• Lymphoma and Multiple myeloma patients in remission could still be considered to have the disease and should be assigned their
appropriate primary neoplasm code (C90-C96), except Hodgkin lymphomas which after certain time in remission, are considered cured
and should be coded as Z75.81: Personal history of Hodgkin's lymphoma.*
[28], [29], [30]
103
CDI Tips
HCC 11 – HCC 12
• Behavior: malignant, neuroendocrine, carcinoma in situ, benign, or unknown.
• Metastasis (first code primary site then secondary cancer/metastatic site if applicable)
•If primary malignancy has been successfully treated and there is no further evidence of active disease, Code First: the
secondary malignancy and assign a personal history code from category Z85.XX to indicate the former site of
malignancy as secondary code
• Morphology: histological type, stage, grade.
• Anatomic site: where is located.
• Laterality: left, right, bilateral.
• Review Hematology/Oncology consult notes to locate the specific description and status of the severe cancer to assign the
most appropriate code.
Continue using active/current diagnosis and documenting in the Assessment/Plan if patient:
• Is currently undergoing surgery, radiotherapy, immunotherapy, targeted therapy or chemotherapy, this should be reflected
in Plan/Assessment of Office visit to properly validate active diagnosis.
• Current Adjuvant therapy status post excision of the neoplasm, this should be reflected in Plan/Assessment of Office visit
to properly validate active diagnosis.
• Example: Malignant neoplasm of right breast, unspecified site C50.911 Patient is s/p excision of breast cancer. She
has completed chemotherapy, radiotherapy, and is now on hormone therapy for 5 years.
• Active surveillance, meaning that the Oncologist explained the different therapeutic options and the patient/caregiver
refused any treatment, thus the provider keeps the patient in active surveillance to evaluate the progress of the chronic
disease. [31]
104
CDI Tips
• Breast cancer:
• If patient is on Anastrozole or Tamoxifen (hormonal-based chemotherapy), condition must be
coded as active Breast cancer.
• If treatment is completed, the cancer is considered INACTIVE/HISTORY.
• Prostate cancer:
• If seeds were placed, condition can be coded as active Prostate cancer up to 6 months after last
radiation.
• If patient is on Lupron, if medication is still active, condition must be coded as active Prostate
cancer.
PSA follow-ups after patient is in
remission is not considered
active surveillance.
105
CDI Tips
Common Coding Opportunities
• Disorders of Immunity [HCC 47]
• D84.81: Immunodeficiency due to conditions classified elsewhere, such
as: Chromosomal abnormalities (Q90-Q99), malignant neoplasms • D84.822: Immunodeficiency due to external
(C00-C96). RA, LUPUS, Ulcerative colitis, Crohn’s disease, Cirrhosis, causes.
Multiple myeloma, Diabetes with hyperglycemia and evidence of • Use additional code for external cause
opportunistic infection. Extreme PCM, Moderate to severe COPD with such as: Exposure to ionizing radiation
evidence of several exacerbations during the year. (W88), Transplants (Z94.XX),
• EXCLUDES: HIV disease (B20). Radiological procedure or Radiotherapy
(Y84.2).
• D84.821: Immunodeficiency due to drugs, including but not limited to:
immunosuppressants, anti-monoclonal, long-term use of corticosteroids
(Prednisone), DMARDs (hydroxychloroquine, methotrexate), anti-TNF,
and chemotherapy.
• Use additional code to identify:
o Adverse effect of drug (T36-T50 with 5th or 6th character 5)
o Associated long term (current) therapy drug or medication such
as: Long term (current) drug therapy systemic steroids, other long
term (current) drug therapy (Z79.899) which includes
106 chemotherapy and/or immunotherapy.
Diseases and disorders of the nervous system
Most Common Codes
HCC Description RAF
70 Quadriplegia 1.242
71 Paraplegia 1.068
74 Cerebral Palsy 0.339
75 Myasthenia Gravis/Myoneural disorders inflammatory and toxic 0.472
neuropathy
77 Multiple sclerosis 0.423
78 Parkinson’s and Huntington's disease 0.606
79 Seizures disorders and convulsions 0.220
103 Hemiplegia/hemiparesis 0.437
104 Monoplegia, other paralytic syndromes 0.331
Refer to most current ICD 10 mapping to find the most
108 specific diagnosis code.
HCC 75: Polyneuropathy
109
G63: Polyneuropathy in diseases classified elsewhere
• Code First underlying disease i.e.:
• Amyloidosis (E85.-)
• Endocrine disease, except diabetes (E00-E07, E15-E16, E20-E34)
• Metabolic diseases (E70-E88)
• Neoplasm (C00-D49)
• Nutritional deficiency (E40-E64)
• Excludes:
• Polyneuropathy (In):
• Diabetes Mellitus (E08-E13 With .42)
DO NOT use G63 code in
• Diphtheria (A36.83) patient with diabetes. Instead,
• Infectious Mononucleosis (B27.0-b27.9 With 1)
• Lyme Disease (A69.22)
consider: E11.42: type 2
• Mumps (B26.84) diabetes with polyneuropathy.
• Postherpetic (B02.23)
• Rheumatoid Arthritis (M05.5-)
• Scleroderma (M34.83)
• Systemic Lupus Erythematosus (M32.19)
110
Importance of Foot Exams
• Foot exams should not be restricted solely to Frequency = Yearly
diabetic patients. Other conditions that may
warrant a foot exam include:
• Hypothyroidism (E03.9)
• Vitamin B12 deficiency (D51.9)
• Alcohol abuse or dependence (F10.10,
F10.20 or F10.21)
• History of Chemotherapy/Radiation (Z92.21
or Z92.3)
• Certain medications use can cause
neuropathy, such as Metronidazole,
amiodarone, etc.
111
G62.0: Drug-Induced Polyneuropathy
[33]
112
M05.5XX: Rheumatoid
polyneuropathy with
rheumatoid arthritis
• In patients with confirmed
rheumatoid arthritis and
polyneuropathy due to RA, do
not use G63 code, use
instead M05.5XX.
HCC 40 + HCC 75
113
HCC 79: Seizure Disorder and Convulsion:
Document: ICD 10 Code Description HCC
• Current treatment Generalized idiopathic epilepsy and epileptic
• Date of last episode, and any G40.309 syndromes, not intractable, without status 79
complications if applies epilepticus
• Recurrence of episodes Other epilepsy, not intractable, without status
G40.802 79
• Review specialist (neurology) epilepticus
consult notes to locate the specific G40.89 Other seizures 79
description and status of the
disease to assign the most Epilepsy, unspecified, not intractable, without
appropriate code. G40.909 79
status epilepticus
R56.1 Post traumatic seizures 79
R56.9 Unspecified convulsions 79
114
Ophthalmological Disorders
Most Common Codes
ICD 10 Code Description HCC HCC 122 – RAF Score= 0.222
Code HCC 124 – RAF Score= 0.521
H35.32XX Exudative (WET) age-related macular
124
degeneration
HCC 122: Total of 124 ICD 10 Codes
E10.35XX
Type 1 diabetes mellitus with proliferative HCC 124: Total of 16 ICD 10 Codes
122
diabetic retinopathy
E11.35XX
Type 2 diabetes mellitus with proliferative Common records to review:
122
diabetic retinopathy
Eye exam, Optometrist note,
Ophthalmology consultation
116
Transplant status
Most Common Codes
ICD 10 Code Code Description HCC
HCC 186 – RAF Score= 0.832
Z94.1 Heart transplant status 186
HCC 186: Total of 48 ICD 10 Codes
Z94.2 Lung transplant status 186
Common records to review:
Z94.3 Heart and lungs transplant status 186
Previous PCP records, ER/ED records,
Z94.4 Liver transplant status 186 Surgery records, Oncology records.
Z94.81 Bone marrow transplant status 186
Z94.82 Intestine transplant status 186
Z94.83 Pancreas transplant status 186
Z94.84 Stem cells transplant status 186
Z95.811 Presence of heart assist device 186 Kidney transplant does not Risk Adjust as of Feb.
Z95.812
Presence of fully implantable artificial
186
2019, but is applicable for immunodeficiency
heart
codes and CKD codes if present
118
Additional Tips for Coding Opportunities
HCC 28: K70.3X: Alcoholic cirrhosis of liver
Liver Biopsy
or Elastography are
considered diagnostic tests
for hepatic cirrhosis.
120
New V28 model
New V28 model
122
New V28 model
123
Asthma in V28 model
Asthma:
Code Description RAF HCC
Score
J4550 Severe persistent asthma, uncomplicated 0.818 279
J4551 Severe persistent asthma with (acute) exacerbation 0.818 279
J4552 Severe persistent asthma with status asthmaticus 0.818 279
Asthma is considered severe persistent if any or all the following are true:
Documentation is key:
•Symptoms occur several times daily. ROS, physical exam,
assessment and plan
•Nighttime symptoms are frequent, often nightly.
(Medication).
•Rescue inhalers are used several times daily.
•Asthma symptoms severely impair your ability to function normally.
•Lung function is less than 60% of the predicted value.
124
Other new HCC in V28 model
Hepatic/Alcoholic conditions:
Code Description RAF Score HCC
J910 Malignant pleural effusion 4.209 17
K7010 Alcoholic hepatitis without ascites 0.185 65
K7011 Alcoholic hepatitis with ascites 0.185 65
K713 Toxic liver disease with chronic persistent hepatitis 0.185 65
K714 Toxic liver disease with chronic lobular hepatitis 0.185 65
K7150 Toxic liver disease with chronic active hepatitis without ascites 0.185 65
K7151 Toxic liver disease with chronic active hepatitis with ascites 0.185 65
K717 Toxic liver disease with fibrosis and cirrhosis of liver 0.447 64
125
Other new HCC in V28 model
Diabetes additional codes:
Code Description RAF Score HCC
E113212 Type 2 diabetes mellitus with mild nonproliferative diabetic retinopathy with macular edema, left eye 0.336 298
E113213 Type 2 diabetes mellitus with mild nonproliferative diabetic retinopathy with macular edema, bilateral 0.336 298
E113219 Type 2 diabetes mellitus with mild nonproliferative diabetic retinopathy with macular edema, unspecified eye 0.336 298
E113311 Type 2 diabetes mellitus with moderate nonproliferative diabetic retinopathy with macular edema, right eye 0.336 298
E113312 Type 2 diabetes mellitus with moderate nonproliferative diabetic retinopathy with macular edema, left eye 0.336 298
E113313 Type 2 diabetes mellitus with moderate nonproliferative diabetic retinopathy with macular edema, bilateral 0.336 298
E113319 Type 2 diabetes mellitus with moderate nonproliferative diabetic retinopathy with macular edema, unspecified eye 0.336 298
E113411 Type 2 diabetes mellitus with severe nonproliferative diabetic retinopathy with macular edema, right eye 0.336 298
126
Other new HCC in V28 model
Artificial leg:
Code Description RAF HCC
Score
Z9713 Presence of artificial right leg (complete) (partial) 0.598 409
Z9714 Presence of artificial left leg (complete) (partial) 0.598 409
Z9716 Presence of artificial legs, bilateral (complete) (partial) 0.598 409
Others: Benign carcinoid tumors, Anorexia/Bulimia nervosa.
127
References
1. Extracted from: "Report to Congress – Medicare Advantage Risk Adjustment - December 2021" Available at: https://www.cms.gov/files/document/report-congress-
risk-adjustment-medicare-advantage-december-2021.pdf
2. Watson, Monica M. Documentation and Coding Practices for Risk Adjustment and Hierarchical Condition Categories. Journal of AHIMA 89, no.6 (June 2018): extended
online version. Available at: https://bok.ahima.org/doc?oid=302516
3. Heidenreich PA, Bozkurt B, Aguilar D, Allen LA, Byun JJ, Colvin MM, Deswal A, Drazner MH, Dunlay SM, Evers LR, Fang JC, Fedson SE, Fonarow GC, Hayek SS, Hernandez
AF, Khazanie P, Kittleson MM, Lee CS, Link MS, Milano CA, Nnacheta LC, Sandhu AT, Stevenson LW, Vardeny O, Vest AR, Yancy CW. 2022 AHA/ACC/HFSA guideline for the
management of heart failure: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation.
2022;145:e895–e1032. doi: 10.1161/CIR.0000000000001063
4. McKee PA et. al. The natural history of congestive heart failure: the Framingham study. New England Journal of Medicine 1971;285:1441–6
5. Malik A, Brito D, Vaqar S, et al. Congestive Heart Failure. [Updated 2022 Nov 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available
from: https://www.ncbi.nlm.nih.gov/books/NBK430873/
6. Maeder, M. T., Weber, L., Buser, M., Gerhard, M., Haager, P. K., Maisano, F., & Rickli, H. (2018). Pulmonary Hypertension in Aortic and Mitral Valve Disease. Frontiers in
cardiovascular medicine, 5, 40. https://doi.org/10.3389/fcvm.2018.00040
7. Senst B, Tadi P, Basit H, et al. Hypercoagulability. [Updated 2022 Sep 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available
from: https://www.ncbi.nlm.nih.gov/books/NBK538251/
8. Povsic, T. J., Henry, T. D., & Ohman, E. M. (2021). Therapeutic Approaches for the No-Option Refractory Angina Patient. Circulation. Cardiovascular interventions, 14(2),
e009002. https://doi.org/10.1161/CIRCINTERVENTIONS.120.009002
128
References
9. Collet, J. P., Thiele, H., Barbato, E., Barthélémy, O., Bauersachs, J., Bhatt, D. L., Dendale, P., Dorobantu, M., Edvardsen, T., Folliguet, T., Gale, C. P., Gilard, M., Jobs, A., Jüni,
P., Lambrinou, E., Lewis, B. S., Mehilli, J., Meliga, E., Merkely, B., Mueller, C., … ESC Scientific Document Group (2021). 2020 ESC Guidelines for the management of acute coronary
syndromes in patients presenting without persistent ST-segment elevation. European heart journal, 42(14), 1289–1367. https://doi.org/10.1093/eurheartj/ehaa575
10. European Stroke Organisation, Tendera, M., Aboyans, V., Bartelink, M. L., Baumgartner, I., Clément, D., Collet, J. P., Cremonesi, A., De Carlo, M., Erbel, R., Fowkes, F. G., Heras,
M., Kownator, S., Minar, E., Ostergren, J., Poldermans, D., Riambau, V., Roffi, M., Röther, J., Sievert, H., … ESC Committee for Practice Guidelines (2011). ESC Guidelines on the
diagnosis and treatment of peripheral artery diseases: Document covering atherosclerotic disease of extracranial carotid and vertebral, mesenteric, renal, upper and lower
extremity arteries: the Task Force on the Diagnosis and Treatment of Peripheral Artery Diseases of the European Society of Cardiology (ESC). European heart
journal, 32(22), 2851–2906. https://doi.org/10.1093/eurheartj/ehr211
11. Global Initiative for Chronic Obstructive Lung Disease (2023)POCKET GUIDE TO COPD DIAGNOSIS, MANAGEMENT, AND PREVENTION A Guide for Health Care Professionals, p. 5,
para. 5 Available at: https://goldcopd.org/2023-gold-report-2/
12. Mejza, F., Gnatiuc, L., Buist, A. S., Vollmer, W. M., Lamprecht, B., Obaseki, D. O., Nastalek, P., Nizankowska-Mogilnicka, E., Burney, P. G. J., BOLD collaborators, & BOLD study
collaborators (2017). Prevalence and burden of chronic bronchitis symptoms: results from the BOLD study. The European respiratory journal, 50(5),
1700621. https://doi.org/10.1183/13993003.00621-2017
13. Dretzke J, Blissett D, Dave C, et al. The cost-effectiveness of domiciliary non-invasive ventilation in patients with end-stage chronic obstructive pulmonary disease: a systematic
review and economic evaluation. Southampton (UK): NIHR Journals Library; 2015 Oct. (Health Technology Assessment, No. 19.81.) Chapter 1, Background. Available from:
https://www.ncbi.nlm.nih.gov/books/NBK321580/
14. American Diabetes Association Professional Practice Committee; 2. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes—2022. Diabetes Care 1 January
2022; 45 (Supplement_1): S17–S38. https://doi.org/10.2337/dc22-S002
15. Chen TK, Knicely DH, Grams ME. Chronic Kidney Disease Diagnosis and Management: A Review. JAMA. 2019;322(13):1294–1304. doi:10.1001/jama.2019.14745
16. Pop-Busui, R., Boulton, A. J., Feldman, E. L., Bril, V., Freeman, R., Malik, R. A., Sosenko, J. M., & Ziegler, D. (2017). Diabetic Neuropathy: A Position Statement by the American
Diabetes Association. Diabetes care, 40(1), 136–154. https://doi.org/10.2337/dc16-2042
129
References
17. Jensen, G.L., Cederholm, T., Correia, M.I.T.D., Gonzalez, M.C., Fukushima, R., Higashiguchi, T., de Baptista, G.A., Barazzoni, R., Blaauw, R., Coats, A.J.S., Crivelli, A., Evans, D.C.,
Gramlich, L., Fuchs-Tarlovsky, V., Keller, H., Llido, L., Malone, A., Mogensen, K.M., Morley, J.E., Muscaritoli, M., Nyulasi, I., Pirlich, M., Pisprasert, V., de van der Schueren, M., Siltharm,
S., Singer, P., Tappenden, K.A., Velasco, N., Waitzberg, D.L., Yamwong, P., Yu, J., Compher, C. and Van Gossum, A. (2019), GLIM Criteria for the Diagnosis of Malnutrition: A Consensus
Report From the Global Clinical Nutrition Community. Journal of Parenteral and Enteral Nutrition, 43: 32-40. https://doi.org/10.1002/jpen.1440
18. Purnell JQ. Definitions, Classification, and Epidemiology of Obesity. [Updated 2023 May 4]. In: Feingold KR, Anawalt B, Blackman MR, et al., editors. Endotext [Internet]. South
Dartmouth (MA): MDText.com, Inc.; 2000-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK279167/
19. Wissam Saliba, Boutros El-Haddad. Secondary Hyperparathyroidism: Pathophysiology and Treatment. The Journal of the American Board of Family Medicine Sep 2009, 22 (5) 574-
581; DOI: 10.3122/jabfm.2009.05.090026
20. Dominguez A, Muppidi V, Gupta S. Hyperaldosteronism. [Updated 2023 Feb 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from:
https://www.ncbi.nlm.nih.gov/books/NBK499983/
21. Sellos-Moura, M., Glavin, F., Lapidus, D., Evans, K., Lew, C. R., & Irwin, D. E. (2020). Prevalence, characteristics, and costs of diagnosed homocystinuria, elevated homocysteine, and
phenylketonuria in the United States: a retrospective claims-based comparison. BMC health services research, 20(1), 183. https://doi.org/10.1186/s12913-020-5054-5
22. Pillai AA, Fazal S, Mukkamalla SKR, et al. Polycythemia. [Updated 2023 May 20]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available
from: https://www.ncbi.nlm.nih.gov/books/NBK526081/
23. Hasin DS, Sarvet AL, Meyers JL, et al. Epidemiology of Adult DSM-5 Major Depressive Disorder and Its Specifiers in the United States. JAMA Psychiatry. 2018;75(4):336–346.
doi:10.1001/jamapsychiatry.2017.4602
24. Shaji, K. S., Sivakumar, P. T., Rao, G. P., & Paul, N. (2018). Clinical Practice Guidelines for Management of Dementia. Indian journal of psychiatry, 60(Suppl 3), S312–S328.
https://doi.org/10.4103/0019-5545.224472
25. Grant, B. F., Saha, T. D., Ruan, W. J., Goldstein, R. B., Chou, S. P., Jung, J., Zhang, H., Smith, S. M., Pickering, R. P., Huang, B., & Hasin, D. S. (2016). Epidemiology of DSM-5 Drug Use
Disorder: Results From the National Epidemiologic Survey on Alcohol and Related Conditions-III. JAMA psychiatry, 73(1), 39–47.
130
References
26. Addicott M. A. (2014). Caffeine Use Disorder: A Review of the Evidence and Future Implications. Current addiction reports, 1(3), 186–192.
https://doi.org/10.1007/s40429-014-0024-9
27. Jahan AR, Burgess DM. Substance Use Disorder. [Updated 2023 Apr 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available
from: https://www.ncbi.nlm.nih.gov/books/NBK570642/
28. Potre, O., Pescaru, M., Sima, A., Ionita, I., Tudor, R., Borsi, E., Samfireag, M., & Potre, C. (2021). Evaluation of the Relapse Risk and Survival Rate in Patients with
Hodgkin Lymphoma: A Monocentric Experience. Medicina (Kaunas, Lithuania), 57(10), 1026. https://doi.org/10.3390/medicina57101026
29. Thandra, K. C., Barsouk, A., Saginala, K., Padala, S. A., Barsouk, A., & Rawla, P. (2021). Epidemiology of Non-Hodgkin's Lymphoma. Medical sciences (Basel,
Switzerland), 9(1), 5. https://doi.org/10.3390/medsci9010005
30. Sonneveld P. (2017). Management of multiple myeloma in the relapsed/refractory patient. Hematology. American Society of Hematology. Education
Program, 2017(1), 508–517. https://doi.org/10.1182/asheducation-2017.1.508
31. Shill, D. K., Roobol, M. J., Ehdaie, B., Vickers, A. J., & Carlsson, S. V. (2021). Active surveillance for prostate cancer. Translational andrology and urology, 10(6),
2809–2819. https://doi.org/10.21037/tau-20-1370
32. Hanewinckel, R., van Oijen, M., Ikram, M. A., & van Doorn, P. A. (2016). The epidemiology and risk factors of chronic polyneuropathy. European journal of
epidemiology, 31(1), 5–20. https://doi.org/10.1007/s10654-015-0094-6
33. Jones, M. R., Urits, I., Wolf, J., Corrigan, D., Colburn, L., Peterson, E., Williamson, A., & Viswanath, O. (2020). Drug-Induced Peripheral Neuropathy: A Narrative
Review. Current clinical pharmacology, 15(1), 38–48. https://doi.org/10.2174/1574884714666190121154813
131
References
34. American Academy of Family Physicians. (n.d.). Hierarchical Condition Category. Retrieved May 2023, from https://www.aafp.org/family-physician/practice-and-
career/getting-paid/coding/hierarchical-condition-category.html
35. ICD10Data.com. (n.d.). ICD-10 Data. Retrieved May 2023, from https://www.icd10data.com/
36. Centers for Medicare & Medicaid Services. (2023, January 11). FY 2023 ICD-10-CM Coding Guidelines. Retrieved May 2023, from
https://www.cms.gov/files/document/fy-2023-icd-10-cm-coding-guidelines-updated-01/11/2023.pdf
128
Thank you
You might also like
- PLABable Vs MedRevisions: Check The Sample Notes UKMLA and PLAB Exam - Cardiology Notes Updated - MedrevisionNo ratings yetPLABable Vs MedRevisions: Check The Sample Notes UKMLA and PLAB Exam - Cardiology Notes Updated - Medrevision32 pages
- To Mitigate Transition of HCC Mapping (V24-V28)No ratings yetTo Mitigate Transition of HCC Mapping (V24-V28)94 pages
- Katz - HCC-RAF Diagnosis Coding - PCP - 08-26-2020No ratings yetKatz - HCC-RAF Diagnosis Coding - PCP - 08-26-202066 pages
- The Role of Hccs in A Value-Based Payment SystemNo ratings yetThe Role of Hccs in A Value-Based Payment System7 pages
- Mips Tips Oct. 2018 - What Is HCC and How Does It Impact 10.16.18 FinalNo ratings yetMips Tips Oct. 2018 - What Is HCC and How Does It Impact 10.16.18 Final39 pages
- ChenEllisToroAsh Medicare-Risk-Adjustment-Models 20131231 2No ratings yetChenEllisToroAsh Medicare-Risk-Adjustment-Models 20131231 222 pages
- 2024 Centene MRA Coding Guidelines Playbook 8.2.2024No ratings yet2024 Centene MRA Coding Guidelines Playbook 8.2.202462 pages
- Medicare Advantage Transition Brings Big Changes to Risk Adjustment CodingNo ratings yetMedicare Advantage Transition Brings Big Changes to Risk Adjustment Coding5 pages
- HEDIS Documentation Coding Guide-Adult 2020 - 900-3807A-0819 Approved 9.6rev10.21No ratings yetHEDIS Documentation Coding Guide-Adult 2020 - 900-3807A-0819 Approved 9.6rev10.2110 pages
- Apixio-APM-Guide-to-Risk-Adjustment-051 MoodNo ratings yetApixio-APM-Guide-to-Risk-Adjustment-051 Mood12 pages
- The Science of HCC Documentation and CodingNo ratings yetThe Science of HCC Documentation and Coding20 pages
- 2023 Benefit Year Final HHS Risk Adjustment Model CoefficientsNo ratings yet2023 Benefit Year Final HHS Risk Adjustment Model Coefficients18 pages
- ALL CARE MR RiskAdjustmentMedRecordTips Mrdcoding TipsNo ratings yetALL CARE MR RiskAdjustmentMedRecordTips Mrdcoding Tips2 pages
- Clinical Documentation in The Inpatient SettingNo ratings yetClinical Documentation in The Inpatient Setting30 pages
- ICD-10 HIPAA5010 (A Joint Presentation)No ratings yetICD-10 HIPAA5010 (A Joint Presentation)77 pages
- Final 2021 Benefit Year Final HHS Risk Adjustment Model CoefficientsNo ratings yetFinal 2021 Benefit Year Final HHS Risk Adjustment Model Coefficients26 pages
- Textbook of Urgent Care Management: Chapter 38, Audits by Managed-Care Organizations and Regulatory AgenciesFrom EverandTextbook of Urgent Care Management: Chapter 38, Audits by Managed-Care Organizations and Regulatory AgenciesNo ratings yet
- Pharmacology of Inotropes and Vasopressors100% (1)Pharmacology of Inotropes and Vasopressors51 pages
- Assessment of Dry Weight in Hemodialysis: An Overview: ReviewNo ratings yetAssessment of Dry Weight in Hemodialysis: An Overview: Review12 pages
- Risk For Decreased Cardiac Output: Nursing Diagnosis100% (1)Risk For Decreased Cardiac Output: Nursing Diagnosis4 pages
- Aegon Life Ci Care Rider: A Non Linked Critical Illness RiderNo ratings yetAegon Life Ci Care Rider: A Non Linked Critical Illness Rider13 pages
- Full download Practical Cardiology Evaluation 2nd Edition Baker pdf docx100% (11)Full download Practical Cardiology Evaluation 2nd Edition Baker pdf docx60 pages
- Heart Failure: Definition and EpidemiologyNo ratings yetHeart Failure: Definition and Epidemiology6 pages
- Etiology and Management of Edema A ReviewNo ratings yetEtiology and Management of Edema A Review14 pages
- The Silent Storm: Understanding HypertensionNo ratings yetThe Silent Storm: Understanding Hypertension11 pages